Anti-Protease sorbent "Hemo-proteazsorb"
This imbalance is the result of a massive release of cellular proteases, activation of cellular proteolytic systems, and decrease of protease inhibitors concentration. Application of the multivalent protease inhibitors such as aprotinin and its analogues in this case is theoretically sound, however these drugs may damage the protease-mediated regulation of various physiological processes.
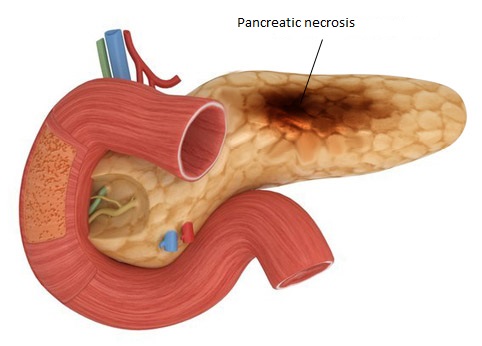
Pathogenesis of systemic abnormalities during pancreatitis is associated with a high concentration of pancreatic proteases in the blood, which reduce activation of the blood proteolytic systems. Alteration of the balance between proteases and their natural inhibitors is a trigger of endogenous intoxication syndrome, which controls disease severity and the clinical outcome. Therefore, drugs which act as inhibitors of proteases are an important component of a complex treatment of acute pancreatitis.
A high fatality rate associated with this disease suggests that the effectiveness of conservative and surgical treatment is not sufficient in the case of acute pancreatitis. New methods of extracorporeal detoxification using hemoperfusion over carbon sorbents has made it possible to improve the outcome of pancreatitis treatment. However, hemosorption leads to only a transient decrease in blood proteolytic activity and does not correct the imbalance in the protease-inhibitor system, and the carbon hemosorbents are nonspecific. The development and application of anti-protease hemosorbents with specific bioligands therefore has potential in pancreatitis treatment.
We have developed an efferent method for correction of hyperproteasemia, which is based on elimination of active proteases from blood by means of biospecific hemosorption. A new generation of biospecific anti-protease hemosorbents have been developed with the use of ovomucoid immobilized in a polyacrylamide gel. Ovomucoid is a highly glycosylated protein abundant in hen's egg white, with a molecular weight of 28 kD. The ovomucoid ligand inhibits serine proteases very effectively. Here we present medical and biological studies and results of clinical trials of the anti-protease hemosorbent "Hemo-proteazsorb"—> which has been previously tested in dogs and a small number of patients.
431 randomly chosen patients treated for destructive-pancreatitis in surgical departments of Minsk, Belarus, hospitals, were studied. The diagnosis was based on the clinical symptoms and amylase level (>1,000 UL-1) and was verified during laparoscopy or laparotomy. All patients were treated with conservative and surgical methods. Direct hemosorption (HS) was used after an adequate correction of circulatory injury was reached. HS was carried out for 100 min, at the blood flow rate of 60-80 mLmin-1, and general intravenous hyalinization (Heparin, Gedeon Richter, Hungary, 0.5 mgkg-1 of body mass) was performed. The vein-venous mode of hemoperfusion was used with subclavian, basilic or femoral veins. The anti-protease sorbent "Hemo-proteazsorb" (80 mL) was used in an extracorporeal plastic column. The time interval between successive HS sessions (from 4 h to 2 days) and the number of sessions were determined in each specific case in accordance with the character and extent of generalization of the inflammatory process in the pancreas and abdominal cavity, severity of endogenous intoxication, and therapeutic effect of the previous sessions.
The fatality rate was also analyzed in the group of 97 randomly-selected patients with acute pancreatitis, treated in Minsk hospitals by a similar treatment program using HS over uncoated activated carbon sorbents of the SKN type. Eighteen healthy donors served as control. It should be noted that patients in both groups were treated with intravenous infusion of the protease inhibitor from bovine lung (Contrykal, Dresden, Germany; 5,000 U per body mass per day).
Total protein, albumin, urea (standard methods) and middle molecules (MM) were determined in citrated plasma. The trypsin-like activity (TLA) of plasma was measured using the chromogenic peptide substrate (Z-glycyl-glycyl-L-arginine-4-nitroanilide). Evaluation of anti-enzymatic potential in plasma was based on concentrations of the main protease inhibitors: α1-proteinase inhibitor (α1-PI) and α2-macroglobulin (α2-M). Student's t-test was used for statistical analysis.
Prior to inclusion of hemosorption in therapy, all patients were in a poor condition due to severe endogenous intoxication and circulatory injury. 376 patients had a stable blood circulation and 64 had a reduced circulation of the blood. All patients had dynamic ileus, and 88 patients had acute multiple organ failure. A special feature of biochemical alterations was imbalance of the protease-inhibitor system. It was manifested in a significant elevation of TLA in blood plasma (P<0.0001) and decrease of α1-PI and α2-M concentrations (P<0.001). The decrease of total protein and albumin, and the increase of urea and MM levels (P<0.001) were also characteristic for protein metabolism injury. The dynamics of biochemical tests in patients treated with HS is presented in Table 1.
Table 1. Biochemical parameters of patient with ADP during hemoperfusion on Hemo-proteazsorb
|
Tests |
Donor |
Patients before HS |
After HS |
Before EU* |
After EU |
One day after HS |
|
TLA (mUL-1) |
14.7 ± 0.4 |
138.6 ± 10.5 |
110.9 ± 8.9 |
133.0± 25.0 |
83.23 ± 8.4 |
68.6±7.6 |
|
α1-PI (UL-1) |
24.6 ± 1.08 |
13.32 ± 1.2 |
16.99± 1.19 |
12.86 ± 2.6 |
13.6 ± 2.7 |
12.5±1.98 |
|
α2-M (UL-1) |
0.53 ± 0.02 |
0.39 ± 0.05 |
0.4 ± 0.06 |
0.43 ± 0.1 |
0.41 ± 0.12 |
0.42±0.04 |
|
Total protein (gL-1) |
82.4 ± 1.6 |
59.6 ± 2.27 |
58.2 ± 2.8 |
69.1 ± 2.4 |
61.9 ± 2.3 |
60.59±1.62 |
|
Albumin (gL-1) |
43.9 ± 0.96 |
26.6 ± 2.03 |
26.8 ± 0.7 |
25.3 ± 1.1 |
28.5 ± 1.3 |
26.1±2.26 |
|
Urea (mmolL-1) |
4.3 ± 0.2 |
9.86 ± 0.8 |
9.3 ± 1.04 |
--------- |
--------- |
7.78±0.74 |
|
MM (gL-1) |
0.53 ± 0.02 |
1.09 ± 0.07 |
0.93 ± 0.07 |
0.94 ± 0.21 |
1.08 ± 0.15 |
0.99±0.06 |
There was a significant decrease of TLA both after blood perfusion through an extracorporeal unit, EU (-39.8 ± 9.6 mUL-1, P < 0.01) and after HS session (-12.8±4.7 mUL-1, P<0.05). Hemosorption over "Hemo-proteazsorb" had no distinct effect on the concentrations of total protein, albumin, urea, MM, α1-PI and α2-M. On the second day after HS, decreases in plasma TLA (-32.8±8.3 mUL-1, P<0.05) and urea (-1.52 ±0.74 mmolL-1, P<0.05) were noted. The level of total protein, albumin, α1-PI and α2-M were not significantly altered.
Within the next several days after hemosorption, reduction of endogenous intoxication, and regression of functional and metabolic disorders in the over whelming majority of patients were observed. These were manifested by increase of motional and intellectual activities, decrease of dyspnea, tachycardia and central venous pressure, and improvement of diuresis. During hemosorption, the peristaltic motions of the gastrointestinal tract appeared or became more intensive leading to meteorism; the loss of water and electrolytes through the gastric tube was diminished. Involution of the inflammatory process in the pancreas was confirmed by decrease of plasma amylase level after hemoperfusion (-240 ±35 UL-1, P<0.001).
The positive therapeutic effect of the complex treatment involving "Hemo-proteazsorb" was achieved in 405 patients and required 2-7 hemosorption sessions. In 46 patients involution of the destructive process in the pancreas was observed after a single procedure of hemosorption. It should be noted that in the process of complex therapy there were no cases in which signs of acute organ system failure appeared or became more intensive. Any purulent complications in or around pancreas were recorded either.
Thus, the fatality rate in the group of patients under study constituted 6.2%. At the same time, the fatality rate in group of patients treated by hemosorption with conventional activated carbon sorbents was much higher (24.7%). The present study shows effectiveness of the biospecific hemosorbent "Hemo-proteazsorb" in the treatment of critically ill patients with destructive pancreatitis. Effectiveness of "Hemo-proteazsorb" is mediated mostly via reduction of endogenous intoxication, functional and metabolic disorders.
We suggest that the extracorporeal elimination of proteases from blood and decrease in the level of toxic and biologically active peptides stimulate endogenous detoxification systems and improve functioning of the compensatory systems in the organism. The clinical effect of "Hemo-proteazsorb" can be attributed to its effect on reduction of proteolytic activity in plasma and, as a result, restoration of the balance between proteases and their inhibitors. Immediately after hemoperfusion, in spite of decrease of the trypsin-like activity, the activity of protease inhibitors in plasma remained its initial low level. This fact is in line with our knowledge on the rates of biosynthesis of these proteins.
